Kala azar means dark pigmentation which is characteristic of cases of visceral leishmaniasis. It is caused by Leishmania donovani bodies and may be present either in endemic, epidemic or sporadic forms.
It is widely prevalent in India in epidemic form in states of Bihar, Assam and Bengal. Kala azar found in East and North Africa is a disease of young children and young adults, being more common in males as compared to females.
Mediterranean region, China, Iran, Arabia, USSR, LATIN America, Bangladesh, Sudan and Ethiopia are other countries where the disease is prevalent. In the Mediterranean region it primarily affects infants and young children and the strain of !eishmania responsible for the disease is often referred to as L. Infantum.
Indian kala azar has clinical picture like that of African form. Humans are the only known reservoirs as compared to other countries where animals like dogs, rodents, jackals and foxes act as reservoirs while animal reservoirs in India are not known. Transmission of the disease is by Sand flies which require humidity, vegetation and heavy rainfall for their development.
Pathology
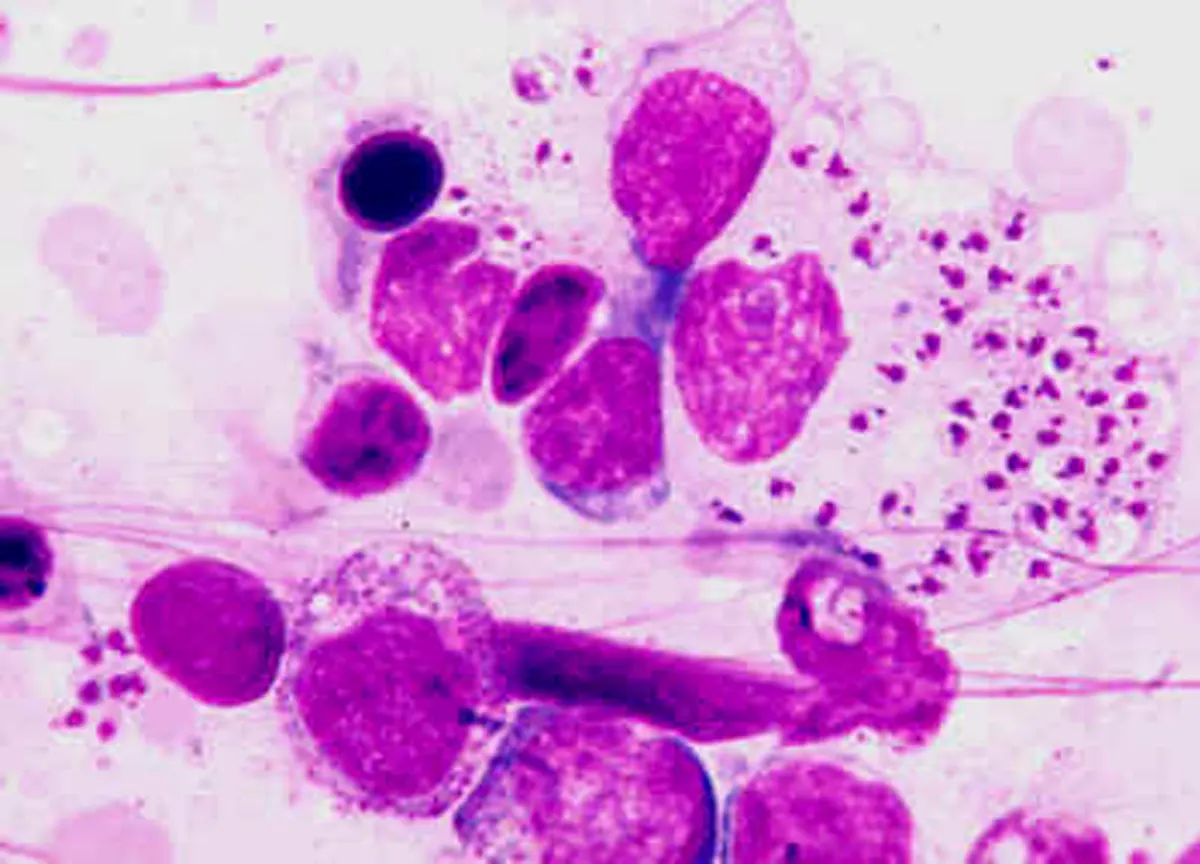
L. Donovani bodies are found in the reticulo endothelial cells of the liver, spleen, bone marrow and skin while in the visceral form the parasites are seen in the macrophages of these organs and produce a humoral immune respone.
In the cutaneous form they appear in macrophages with marked lymphocytic infiltration. The presentation is dependant on the patients cellular response. Both IgG and 1gM immunoglobulins are markedly increased and these contain antibodies against the parasite.
Important changes are seen in spleen, liver and bone marrow. Spleen at first is soft, pulpy and friable and later on an enlaiged spleen becomes hard and fibrous. In chronic cases perislpenitis and infarcts occur. Liver also becomes firm and friable with fatty changes.
In late stages cirrhosis may result. Bone marrow is red and soft with yellow marrow being replaced by red marrow. Lymph glands especially of mesenteric region also become enlarged with central necrosis. But this involvement is more often found in African and Mediterranean varieties than in Indian.
There may be extensive infiltration of the gastrointestinal tract by leishmania leading to malabsorption like picture. A typical leishman lesion consists of plasma cells, histiocytes and lymphocytes along with parasitized macrophages. In some cases immune complex glomerulonephritis and interstitial nephritis may occur.
Clinical picture
Incubation period of the visceral leishmaniasis disease generally ranges from 2-4 months but may occur one to one half year after exposure. The onset often is insidious but in some it may be sudden. Fever may be remittent, intermittent or continuous.
Fever has typical patten. It may be like a case of typhoid, reaching its heights in 1-2 weeks and remains continuous. Subsequently it comes down to normal level by lysis. After a apyrexial stage lasting from weeks upto 2 months, the fever reappears. Fever shows a biphasic character rising daily in the afternoons and evenings. This double rise of fever is characteristic of Kala azar.
Sometimes, the presentation is like that of Malaria, fever coming with rigors and chills almost daily. Very often despite many symptoms, patient feels remarkably well. There is anemia along with rapid loss of weight. Cachexia and emaciation appear along with dark pigmentation of skin.
Spleen enlarges and in great majority it may be the first sign. In the early stages it is soft but not tender. It generally is not palpable before three weeks but within six months it reaches up to the umblius. It now is firm and hard. Liver generally is palpable with a firm lower edge. It is moderately enlarged and non-tender. Cirrhosis of liver and portal hypertension develops in small percentage (10%) of long standing.
Lymphadenopathy of moderate degree may be present but it is more in African Kala Azar. Patients of Kala Azar may have irritating persistent cough and breathlessness. Other features include marked weakness, edema of the limbs, low blood pressure, loss of hair, dry and rough pigmented skin. Abdomen is protuberant because of massive hepato splenomgaly.
Anemia is a very prominent feature. There is pan cytopenia, thromblocytopenia. Leucopenia with a relative increase in lymphocytes and monocytes and decrease in neutrophils and eosinophils. Hemoglobin levels are low. There is autoimmune hemolysis altering the coagulability of blood.
Complications and sequalae
Because of poor body resistance and emaciation of kala azar are more prone to develop infections like pneumonia, Bronchopneumonia and Tuberculosis. Watery diarrhoea and gastro intestinal blood loss are common complications.
Patients with chronic infection develop Amyloidosis, cirrhosis and portal hypertension. Agranulocytosis, Fancytopenia, purpura and epistaxis often develop. Children are more likely to develop cancrum oris.
Patients of fulminant Kala azar are more susceptible to develop AIDS. Following treatment patients of Kala Azar may develop post Kala Azar dermal leishmaniasis in the form of depigmented maculo nodular to wart like lesions over the face and limbs. These generally appear 1 to 2 years after treatment and are important in that they have to be differentiated from leprosy.
Diagnosis
It is based on the clinical profile of the disease and demonstration of L. Donovani bodies in smears taken from Bone marrow, Lymphatic glands, as well as serology and biochemical tests. A case of kala-azar has to be differentiated from typhoid, brucellosis, malaria, tuberculosis, Banti’s disease and leukaemias. Various tests employed to confirm the diagnosis are:
1. Napier’s formal gel or aldehyde test is of considerable value since it is simple bed side test. It is non-specific in nature but is important when it is positive especially in the presence of leucopenia.
2. L. donovani bodies may be demonstrated in buffy coat preparations of blood and bone marrow aspirate. Aspirates taken from enlarged lymph nodes show parasites in 60 percent of cases. Aspirates of spleen or liver may also demonstrate the L. donovani bodies but since there is danger of hemorrhage, aspiration of these organs is not recommended.
3. Oiganisms can be cultured in Nicolle-NovyMacneal (NNN media) media from clinical specimens obtained from splenic or bone marrow aspirates.
4. Antibody detection. Specific sero diagnostic tests are also employed. Conventional methods include gel diffusion, complement fixation test, indirect haem agglutination test, indirect immuno-fluorescent antibody test (IFAT) and counter immuno electro phoresis. Most of these tests have limited sensitivities and specifies.
5. Direct agglutination test (DAT) based on agglutination of the trypsenized whole promastigotes is useful in endemic regions. Its sensitivity ranges from 91-100% and specificity from 72 to 100%.
6. ELISA is an important sero diagnostic tool for leishmaniasis. It is a highly sensitive test and its specificity depends upon the antigen used.
7. A ready to use immuno chromatographic strip test based on rk 39 antigen has been developed as a rapid test for diagnosis of kala azar. An important limitation of this test is the presence of antibodies in healthy controls hailing from endemic regions.
Treatment of Kala Azar
It includes both supportive and curative. All patients of Kala azar should preferably be hospitalized. Any infection complicating the disease be treated by use of proper antibiotics. Nutrition must be maintained. Those with severe anemia may require blood transfusions. Penlavatent antimony compounds are the drug of choice.
Sodium antimony gluconate (Pentostam) is the most commonly used dmg. It is administered J/M or I/V in the dose of 10-20 mg/kg daily for a minimum period of 20 days, Meglumini antimonite is also employed in the dose similar to that of sodium antimony gluconate (20mg/kg I/M) for 40.60 days.
In cases resistant to other antimonials UREA STIBAMINE is given (dose 50-200 mg on alternate days intravenously slowly for 4 weeks. It usually is given along with sodium stibogluconate in resistant cases. Adverse reaction to these compounds include nausea vomiting diarrhoea, giddiness, delirium, jaundice, blood dyscrasias, cardiac toxicity and sudden death.
Pentamidine
It is a diamidine derivative and is a potent leishmanicidae. It is usually reserved for those resistant to antimonial therapy. It is given intra-muscularly in the dose of 4mg/kg three times per week for 5- 25 weeks. Side effects include nausea, vomiting, tachycardia and hypo-tension while systemic toxicity includes hepatotoxicity, leucopenia, thrombocytopenia and development of insulin dependent diabetes.
Hydroxystibamidine
It is another potent drug and is administered intravenously in 250 mg dose daily per 10 days. The course may be repeated after an interval of 2 weeks. Total course is the same as that with Pentamidine. Its toxicity is similar except that it causes late peripheral neuropathy.
Allopurinol
Addition of oral allopurinol in a dose of 20-30 mg/kg per day in three divided doses may help in resistant cases. It has to be given for 6 weeks.
Paromomycin
This aminoglycoside antibiotic has been found useful in resistant cases. Given in the dose of 15-20 mg/kg / day in 3 divided doses I/M daily for 21 days.
In severe cases of kala azar, recombinant human interferon-r has been employed along with antimony salts. Drug resistant kala azar cases may respond to amphotericin B. It probably remains the only drug that can be used. Initially 1mg test dose is injected over 20 mts I.V. followed by 0.3 mg/kg body weight infused over 4-8 hrs. Maximum dose 0.7 mg/kg body weight). Side effects include chills; fever body aches nausea, vomiting, dysponea. Nephrotoxicity and mycorditis.
Miltefosine (Hexadecylphospocho-line) a compound developed originally as anti tumour has been shown to be effective as an oral drug against Kala azar. Dosage 100 mg per day or 50 mg twice a day for 3-4 weeks. Improvement in patient’s condition is noticeable after three days, the fever drops and the patient regains strength. The drug produces a cure rate of 100%. Mother drug sitamaquine or kalazaquine, a b amino quinoloxe has also shown promise as an orally effective agent (dose 1mg/kg/day) for 2 weeks. Side effects with the drugs are nausea, vomiting, loss of appetite, hepatoxicity and nephrotoxicity.
In some cases splenectomy has been carried out with encouraging results.
Prevention of Kala Azar
Control of vector (Sandfly) in endemic areas is an important measure. Insecticides like DDT should be sprayed at regular intervals. Early treatment of cases must be carried out to decrease the morbidity of disease.
Attempts be made to destroy animals like infected dogs to eliminate the reservoir of disease. In endemic areas insect repellants be regularly used and at night one should sleep under fine mosquito net to safe guard against the vector.
Prognosis
It is variable. Early recognition of the disease and prompt adequate treatment is very essential. Death results due to inter current infections and complications like cancrumoris, emaciation, gastrointestinal hemorrhage and malabsorption.
If not treated adequately death occurs within 2 years in 70-85 per cent of cases while in advanced cases mortality is in the range of 15-25 per cent. Where early therapy is instituted and supportive measures are undertaken survival rate is more than 90 per cent.
Post Kala Azar dermal leishmaniasis (PKDL)
After recovery from Kala Azar, a small percentage usually after a period ranging from 6 months to few years, present with macular or erythematous, hypo-pigmented lesions. These are flushed with skin and vary in size from pin head to large lesions.
Common sites are face, extensor surface of limbs and back. A few cases may present with nodular wart like lesions on the chin which may extend on the limbs, trunk and face. These lesions may grow into large tumor like masses. PKDL may persist for a number of years and has to be differentiated from Leprosy and lupus erythematosis.
This is generally considered to be due to presence of L. donovani bodies in the dermis even after the visceral disease has been eliminated. Diagnosis is made by demonstrating LD bodies in the scrapings obtained from skin. Culture on NNN media of aspirate obtained from nodular lesions shall further confirm the diagnosis. Further help can be sought from serological tests.
Treatment of PKDL is on the same lines as that of Kala Azar. If left untreated lesions may ulcerate and’ further worsen the picture. With treatment prognosis is good though a few are left with DE-pigmented areas.
Check out the video below on Kala Azar: